South Africa 2019
14th International Meeting, October 31th - November 2nd
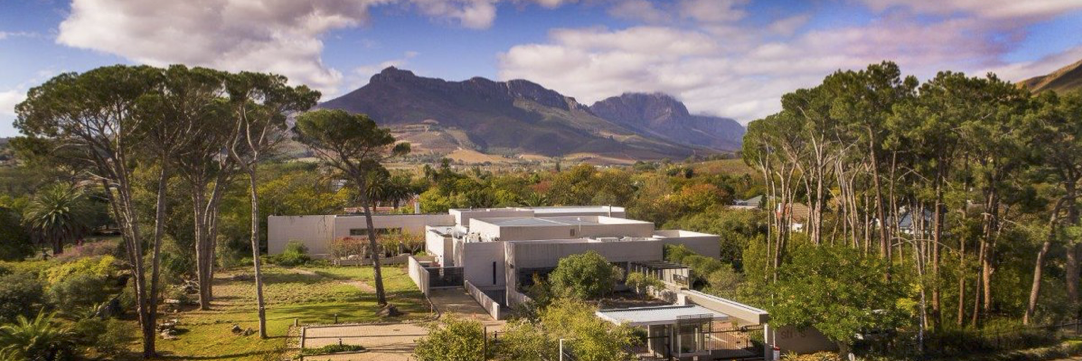
Symposium on Genetics of Movement Disorders in Africa – Report from Capetown, 2 November 2019, STIAS Stellenbosch Conference Centre
On Saturday 2nd November, the Symposium on the Genetics of Movement Disorders in Africa took place at the Stellenbosch Institute for Advanced Studies (STIAS) of the University of Stellenbosch. It was well attended by neurologists, associated healthcare professionals and researchers from all over Africa and the GEoPD consortium members.
Christine Klein spoke about the importance of genetics in movement disorders, as it can help determine appropriate counselling and establish definitive diagnosis. Genetics needs to go global, but large parts of the world are missing, such as Africa and South America, and parts of Asia.
Riaan van Coller (neurologist, Stellenbosch) described profile of Juvenile Onset Parkinsonism of Afrikaan ancestry. He presented age of onset and treatment regimes, and motor feature presentations of five patients.
Jonathan Carr spoke about Genetic testing in South African Population. Over the past 20 years, 700 samples have been analysed. In Morocco for example, the LRRK2 gene is very common, also in the Ashkenazi Jewish population. There is a requirement to take care when making statistics of incidence of genetic populations of PD patients; it will depend on geography and population.
Africa perspectives on genetics of movement disorders was presented by Morenikeji Komolafe (Ile Ife, Nigeria)
In Nigeria, women have less access to healthcare infrastructure, but prevalence of PD is higher in females than in males. PD is quite low incidence in Nigeria, at 10 in 100000. Few patients admit to family history due to stigma or other implications for family members. There are many challenges to care: patients cannot afford drugs, cannot access care, minimal access to health insurance, and negative attitude to genetic testing.
Tanzanian perspectives on genetics of movement disorders – Marieke Dekker, Tanzania
Tanzanian genetics is largely unexplored, therefore presents an opportunity to study untreated advanced PD. PD is diagnosed later or not at all due to delayed referrals and misrecognition, considered by many to be typical of old age. Treatment-naïve patients are seen who don’t fall and don’t freeze, which are interesting features to study. Tanzania needs better infrastructure to develop research: via collaboration to extend local capacity, start using the wealth of information on African genetics.
Why should we know the genetic status of the patient? Mardelle Schoeman, Genetic Counsellor Stellenbosch and Tygerberg hospital
The role and availability of genetic testing for diagnosis has increased dramatically. The value of genetics has diagnostic implication, enables therapeutic options and has impact on treatment. Research remains key to understand conditions better, and inform clinical trial design and future therapies. Genetic counselling is crucial, can help understand diagnosis, inheritance pattern, recurrence risk and psychosocial implications, and help identify family members at risk. Incidentally, predictive testing tends to have low uptake, between 4 and 24%.
GEoPD Consortium – Rejko Krueger
The mission of the GEoPD consortium, founded in 2004, is to develop translational medicine, educate and reach out to develop genetic research in PD. As the longest running consortium for PD, and largest one with continuous membership, it is about sharing the research data to pursue new projects.
GEoPD has developed from a genotyping consortium to one where patients can be pre-selected for clinical trials. It now goes beyond molecular approach into translation. We can do this seamlessly as we have all the expertise. Future opportunities include collaboration with other consortia, clear guidelines and framework, and many mutual benefits to collaboration.
Report on LARGE-PD, PD research consortium in South America: Ignacio Mata
LARGE-PD started in 2006 on a trip to Peru, initially with a collaboration between two sites in Peru and Uruguay that compared incidence of PD in the two populations. Now, have 35 sites in 12 countries. LARGE-PD has almost 4000 samples, with MJFF funding will increase cohort to 9000 by 2021. LARGE-PD created a questionnaire, included clinical data, demographics, environmental exposure to create a database of information across South America. Mentoring programmes are in place for researchers who want to collect and analyse locally. Due to use of cloud, can use pipelines from everywhere to analyse their data.
Matt Farrer – New Developments in the Genetics of PD
Africa is really important to the study of parkinsonism. PD is an umbrella term for many aetiologies. It is polygenic, multifactorial disease, and includes environmental factors.
PD is like a broken engine, where you don’t know what the parts are, how they are integrated or work together! Matt focusses on family based discoveries, looking at late onset PD, through lens of monogenic forms of PD. In population-based discoveries, there are 92 genome loci for PD, primarily known in white Caucasians from Europe and North America.
Panel Discussion:
How do we avoid duplicating errors in the past to move forward with genetics of PD in Africa, and keep the expertise locally in Africa.
Cultural Challenges
In many African countries, people do not want to admit to any health issues in the family. Repeated questioning is required to get any information, it remains a challenge to ascertain heritability of conditions. In countries like Mali, where there are five neurologists for the whole population, people are unwilling to go to hospital and are unaware of PD as a disease and cannot identify if family members had the condition. Often it will take many months for family history to be shared.
Building Capacity
There is a need to build capacity in Africa, upskilling people, training neurologists. Ideally this takes place in Africa, for Africa, as experience in other more developed countries does not easily translate and carries risk losing ownership of the local research projects and data. Currently there is very low healthcare coverage and almost non-existent research facilities in many countries.
Collaboration within consortia such as this are of utmost importance. Mali, for example, has a PD Association that meets every 6 months. 40% of patients come from that.
Not Alone
There are some parallels with Germany 20 years ago, where there were no genetics facilities, in comparison with the USA. This type of technology is developing so fast, and many labs take decision not to invest. Therefore often more constructive to invest in the clinical side, data side and bioinformatics. Then you have the information, with support, and still own it. Genetics infrastructure can often be a poor investment, as the technology is superseded quickly and it gets every less expensive.
Awareness
Awareness campaigns exist in urban Nigeria. In rural areas, there is lack of awareness about existence of conditions like PD. In Mali, young people come to the hospital, but over 60 they find it normal to have some symptoms and stay at home. Secondary diagnosis is very common in Africa, when patients present with an acute condition.
Using the general medical practitioner network is key to inform people about conditions such as PD. In Luxembourg, such outreach has been effective, using internet and radio. This raised awareness, so people now go to the doctor earlier in their experience of symptoms.
The Magic Bean
Lacuna “velvet bean” study will be very interesting to see how the bean can alleviate symptoms, at very low cost. The use of the bean is culturally accepted, thereby changing the everyday situation with the disease.
How to get funding?
Africa needs to upskill itself, if anybody has influence with funding agencies, like Wellcome Trust, MJFF, this would help. Desire to keep the samples in Africa for local research.
ICGBE institution – part of UN. There is one in Trieste and also one in Capetown. One mission is collaboration with other institutions and to help developing countries to develop technology. Could the ICGBE Capetown help here? Can write grants. Research is quicker and more flexible than changing the healthcare system. Tanzania is already collaborating with Trieste
